Eczema Explained: Triggers, Symptoms & Treatments

If your skin often feels dry, itchy, or unpredictable — sometimes flaring overnight for no clear reason — you might be living with eczema. And you’re far from alone.
Eczema (also called atopic dermatitis) affects millions of people worldwide. It’s not just “dry skin” — it’s a complex, chronic condition that can feel frustrating, uncomfortable, and emotional to manage.
The good news? With the right understanding and consistent care, most people can keep their skin calmer and flares less frequent.
This guide walks you through what eczema really is, why it happens, what triggers it, and how to care for your skin with kindness — not harshness.
What Is Eczema?
Eczema is a condition where the skin barrier — the outermost layer that keeps moisture in and irritants out — doesn’t function as strongly as it should.
When that barrier becomes weak, skin loses hydration quickly and reacts to things it would normally tolerate: dry air, soap, fabrics, even stress.
That’s why eczema shows up as dryness, itchiness, and redness. The immune system responds with inflammation, leading to the classic cycle of itch → scratch → more inflammation.
There’s no single cause, and no permanent cure — but understanding your personal triggers and protecting your barrier can dramatically improve comfort and appearance.
Common Symptoms
Eczema looks and feels different from person to person, but common signs include:
- Persistent dryness that doesn’t improve with regular lotion
- Itchy patches that worsen at night or after bathing
- Red, brown, or purple spots (depending on skin tone)
- Rough or scaly texture
- Cracked or oozing areas during flares
- Thickened skin from long-term scratching
It can appear anywhere, but most often affects the elbows, knees, hands, neck, and face. Some people also experience flares on the scalp, eyelids, or body folds.
The Root Causes of Eczema
Eczema develops when several factors overlap: genetics, environment, and immune activity.
1. Genetics
Some people inherit a tendency toward a weaker skin barrier.
The filaggrin (FLG) gene plays a key role — it helps skin cells hold moisture and maintain structure. When this gene doesn’t function properly, skin becomes more porous and sensitive.
Learn more in Is Eczema Genetic?
2. Barrier Dysfunction
Even without genetic issues, repeated irritation (from over-cleansing, low humidity, or harsh products) can wear down the barrier. Once it’s compromised, moisture escapes and inflammation begins.
3. Immune Overreaction
People with eczema often have a heightened immune response. Triggers that wouldn’t bother most skin — like fragrance or pollen — can cause redness, itch, and swelling.
4. Environment & Lifestyle
Cold air, stress, certain fabrics, and even hormonal changes can all worsen symptoms.
That’s why eczema feels unpredictable — it’s not just about what you touch, but also what your body’s experiencing inside.
What Triggers Eczema Flare-Ups
Even with good care, eczema can flare when the barrier gets overwhelmed.
Common triggers include:
- Dry air or sudden weather changes
- Soaps, detergents, and fragrances
- Stress and lack of sleep
- Sweat and heat
- Dust, pollen, and pet dander
- Certain fabrics (like wool)
- Hormonal fluctuations
- Illness or infection
Each person’s list looks different. Keeping a short “flare journal” — noting what happened before symptoms — can help you identify your patterns.
Explore this further in What Triggers Eczema Flare-Ups?
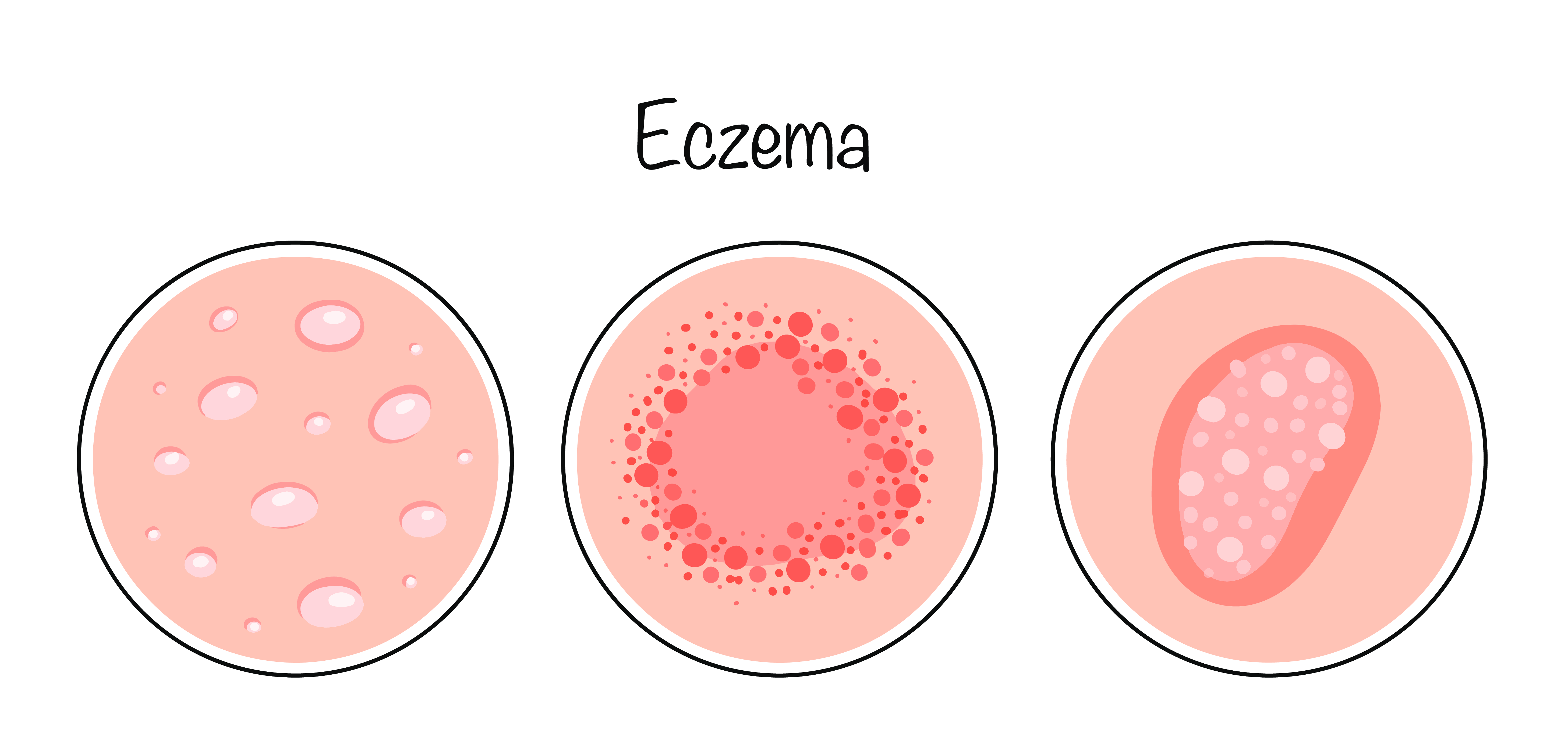
Understanding the Skin Barrier
Think of your skin barrier as a wall made of bricks and mortar.
The “bricks” are your skin cells, and the “mortar” is made of lipids like ceramides and fatty acids.
In eczema, the mortar is often missing or weak — leaving gaps where moisture escapes and irritants sneak in.
That’s why barrier-focused care makes such a difference. Instead of attacking symptoms, it rebuilds what the skin needs to stay resilient.

Everyday Skin Care for Eczema-Prone Skin
You can’t control your genes or the weather, but you can build routines that make your barrier stronger and calmer.
1. Moisturize Consistently
Moisturizer is your first line of defense — not a luxury, but a daily essential.
- Apply a rich, fragrance-free cream or ointment at least twice daily.
- Always moisturize within 30 seconds after bathing.
- Focus on ingredients like ceramides, shea butter, niacinamide, and colloidal oatmeal.
If you’d like more help finding formulas that fit, explore Best Moisturizers for Eczema.
2. Gentle Cleansing
Avoid foaming washes and bar soaps that strip oils.
Use mild, pH-balanced cleansers labeled for sensitive skin, and limit baths to 5–10 minutes in lukewarm water.
3. Soothe, Don’t Scrub
Skip physical scrubs, loofahs, or exfoliating brushes on active eczema.
If you have flaky skin, use soft cloths or a gentle chemical exfoliant only after flares calm down.
4. Protect from Irritants
- Choose soft cotton or bamboo fabrics.
- Use fragrance-free laundry detergents.
- Avoid dryer sheets and fabric softeners if they cause itching.
5. Manage Stress and Sleep
Stress hormones affect inflammation. Regular rest, movement, and mindful breaks all help skin recover faster between flares.
When to Seek Professional Care
You can manage mild eczema at home, but see a dermatologist if:
- The itch is disrupting your sleep or daily life.
- The skin is cracked, weeping, or showing yellow crusts (possible infection).
- Over-the-counter moisturizers aren’t providing relief.
- You’re unsure if it’s eczema or another condition.
A professional can confirm the diagnosis, rule out similar conditions like psoriasis, and discuss additional treatment options.
For a quick comparison, see Eczema vs Psoriasis: Key Differences.
Treatment Options (Non-Prescription & Supportive)
Over-the-counter products can make a noticeable difference when used correctly:
- Barrier creams: Help replace missing lipids and reduce water loss.
- Colloidal oatmeal lotions: Calm irritation and itch.
- Fragrance-free ointments: Lock in hydration overnight.
- Cool compresses: Soothe hot, itchy areas during flares.
Avoid products with alcohol, menthol, or added scents — they can sting or worsen dryness.
If topical steroids or prescription creams are needed, your dermatologist will guide you. Over-the-counter care still supports recovery alongside them.
The Emotional Side of Eczema
Eczema isn’t just skin-deep.
The constant itch, visible patches, and unpredictable flares can affect confidence, sleep, and social comfort. It’s completely normal to feel frustrated or self-conscious.
Remember: eczema isn’t your fault. It’s not caused by poor hygiene or neglect — it’s a medical skin condition that requires patience and gentleness.
Simple habits like mindfulness, deep breathing, and keeping your routine minimal can help ease both stress and symptoms over time.
Living with Eczema Long-Term
Managing eczema is about building resilience, not perfection.
Here are some small shifts that make a big difference:
- Stick to a gentle, consistent routine. Skin loves predictability.
- Introduce new products slowly. Patch test before full use.
- Adjust seasonally. Richer creams in winter, lighter ones in summer.
- Hydrate and eat balanced. Skin health starts from within.
- Track flares. Patterns help you prevent future ones.
Eczema care isn’t about “fixing” your skin — it’s about keeping it supported so you can live comfortably in it.
The Role of Education and Community
Knowledge is empowering.
Strawberry’s mission is to make skincare feel less like trial and error, and more like informed self-care.
Our educational library covers everything from flare management to barrier biology — helping you understand your skin and make gentler choices every day.
You can explore more in-depth reads in our eczema series:
Each one expands on a piece of this puzzle — because calmer skin starts with understanding, not extremes.
The Bottom Line
Eczema is complex, but your care routine doesn’t have to be.
Focus on three core principles:
- Rebuild your barrier with gentle, lipid-rich moisturizers.
- Avoid unnecessary irritants like fragrance, harsh cleansers, and overwashing.
- Stay consistent — your skin improves through habits, not quick fixes.
Small daily acts of care, repeated often, help eczema-prone skin stay comfortable and resilient.
Your skin doesn’t need perfection. It just needs you to show up for it — gently, consistently, and with patience.
References:
- American Academy of Dermatology – Eczema Overview
- National Eczema Association – Understanding Eczema
- National Institutes of Health – Atopic Dermatitis Information
Is eczema the same as dry skin?
Not exactly. While eczema causes dryness, it’s much more than that. Eczema involves inflammation, itch, and a weakened skin barrier, meaning your skin reacts more strongly to irritants, weather, and stress than normal dry skin would.
What causes eczema to start?
Eczema results from a mix of genetic, immune, and environmental factors. Some people inherit a weaker skin barrier, while others develop eczema after repeated irritation or stress. There’s no single cause — but barrier repair and trigger management can greatly reduce flares.
Can eczema go away completely?
Eczema can improve or even disappear for periods, especially with consistent care, but it may return if the skin barrier weakens again. The goal is control, not cure — keeping the skin calm, moisturized, and less reactive over time.
How can I tell if I need to see a dermatologist?
You should seek professional help if:
- The itch disrupts sleep or daily activities.
- The skin cracks, bleeds, or becomes infected.
- Over-the-counter moisturizers and care routines aren’t helping.
A dermatologist can confirm your diagnosis, rule out similar conditions (like psoriasis or fungal infections), and suggest prescription options if needed.





