Keratosis Pilaris Explained: Causes, Symptoms & Treatments

If your skin feels rough and bumpy — especially on your upper arms, thighs, or cheeks — you might have something called keratosis pilaris, or KP for short.
Those tiny bumps can look like goosebumps or small pimples that never seem to go away. They’re harmless, but they can be frustrating and affect how you feel about your skin.
Here’s the comforting truth: KP is common, manageable, and completely normal.
Let’s break down what it is, what causes it, how to calm it, and what actually works when it comes to treatment.
What Is Keratosis Pilaris (KP)?
Keratosis pilaris is a very common skin condition that happens when keratin — a protective protein that helps seal your skin barrier — builds up and blocks the tiny hair follicles.
That blockage creates small, hard bumps that can feel dry or rough to the touch.
They often appear on:
- The backs of the upper arms
- The thighs
- The buttocks
- Sometimes the cheeks or calves
KP isn’t an infection or a rash — it’s just how some skin types renew themselves. It’s more about texture than inflammation.
You might also hear it referred to as “chicken skin” or even “strawberry skin” (especially when the dots are darker and visible after shaving).

What KP Looks and Feels Like
Everyone’s KP looks a little different, but most people notice:
- Tiny, firm bumps that don’t pop
- Mild redness or dry patches around the bumps
- Rough texture, like sandpaper
- Flare-ups that come and go, often worse in winter
The bumps are usually painless, though they can occasionally feel itchy or dry.
What Causes Keratosis Pilaris
The exact cause isn’t fully understood, but it’s believed to involve a mix of genetics, dryness, and skin barrier imbalance.
Here’s what plays a role:
1. Keratin Overproduction
Your body produces extra keratin, which clumps together and blocks follicles.
This is why exfoliation (especially chemical exfoliation) can help — it gently loosens the plugs.
2. Genetics
KP tends to run in families. If your parents or siblings have it, you’re more likely to develop it too.
3. Dry or Sensitive Skin
When your barrier is dry or compromised, keratin plugs are more likely to form.
That’s why moisturizing is the most reliable, long-term treatment.
4. Other Skin Conditions
People with eczema or very dry skin often notice KP alongside it.
The common link? A naturally weaker barrier that struggles to retain moisture.
Who Gets KP
Anyone can have KP, but it’s most common in:
- Teenagers and young adults (due to higher keratin production)
- People with dry, sensitive, or eczema-prone skin
- Those living in cold or low-humidity climates
The good news? KP often improves with age as your skin naturally balances itself out.
If you’re curious about that, read Does KP Go Away With Age?.
Is KP Dangerous?
Not at all. KP is completely harmless. It’s not contagious, it’s not a sign of poor hygiene, and it doesn’t damage your skin long term.
The main issue is cosmetic and comfort-related — texture, dryness, and sometimes mild redness.
Still, it’s worth caring for, because hydrated, smooth skin simply feels better.
You can learn more in Is KP Dangerous?.
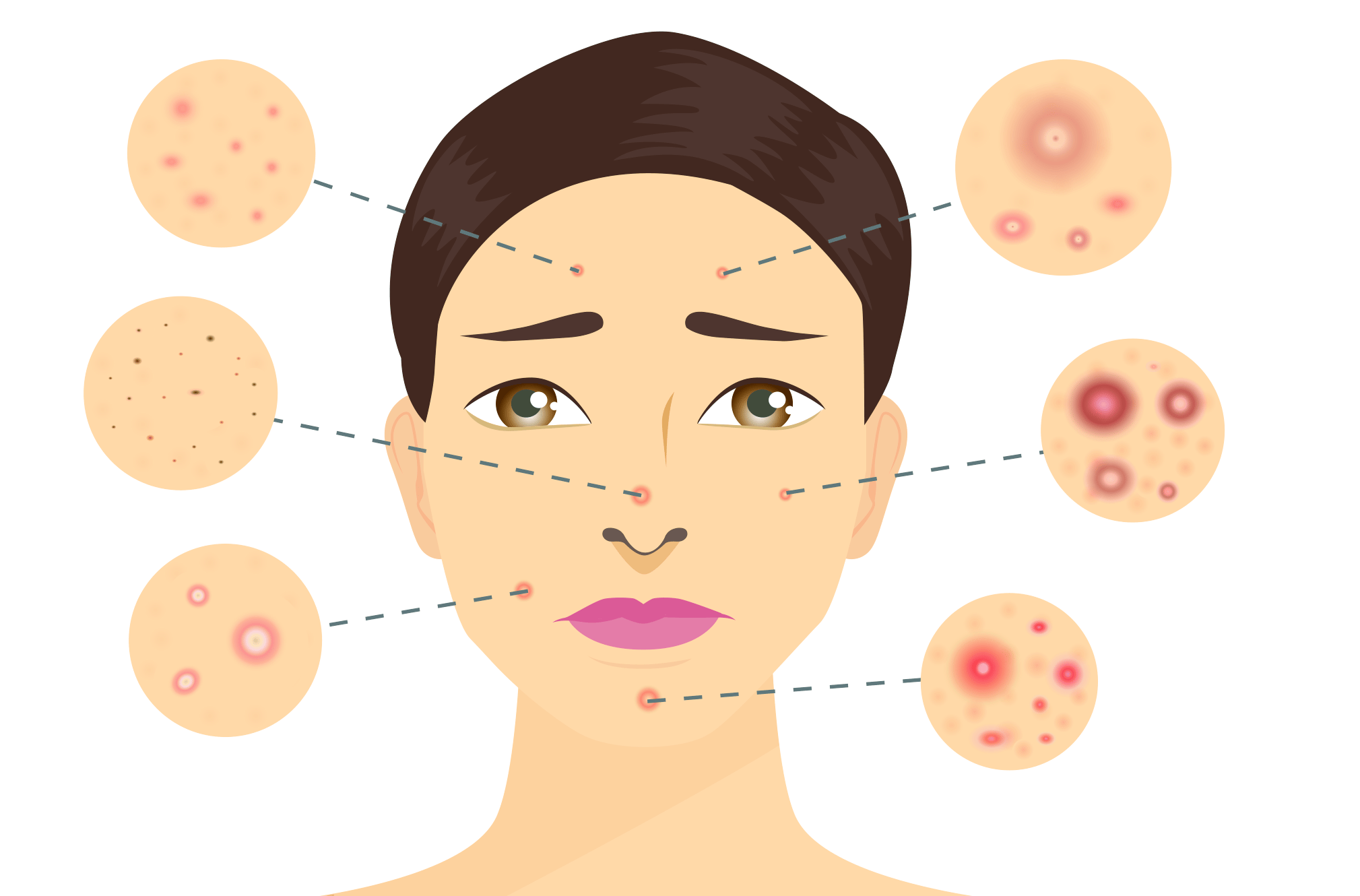
Keratosis Pilaris vs Similar Skin Conditions
KP is often mistaken for other conditions because the bumps look similar.
Here’s how it stands apart:
- KP: Small, firm bumps; not sore; dry texture.
- Eczema: Itchy, inflamed, often red and flaky.
- Acne: Has whiteheads or blackheads; may be painful or pus-filled.
- Folliculitis: Infected follicles; tender and may form clusters.
If you’re not sure what you’re seeing, a dermatologist can confirm it.
Or explore KP vs Eczema vs Acne vs Folliculitis for a deeper visual comparison.

How to Treat KP (What Actually Works)
While there’s no “cure,” KP responds beautifully to gentle, consistent care that focuses on exfoliation, moisture, and barrier repair.
Think of it as a marathon, not a sprint.
1. Gentle Exfoliation
The goal of exfoliation isn’t to scrub the bumps away — it’s to dissolve the keratin plugs that cause them.
The best exfoliants are chemical, not physical.
Lactic acid and urea are the heroes here.
- Lactic acid softens and hydrates while gently renewing the surface.
- Urea breaks down buildup while attracting moisture.
Use them two to three times per week — any more can cause dryness or irritation.
If you’re not sure where to start, read Exfoliation for KP for step-by-step tips.
2. Daily Moisturization
Moisturizer is the single most important step in treating KP.
It keeps the barrier intact, softens rough texture, and reduces the appearance of bumps.
Look for creams that contain:
- Ceramides to rebuild the skin barrier
- Shea butter or squalane for deep nourishment
- Niacinamide to calm redness
- Urea or lactic acid for gentle smoothing
My personal favorite type of KP moisturizer is one that feels rich but still sinks in fast — something built around ceramides and colloidal oatmeal. It keeps skin soft without that heavy film.
Strawberry’s own barrier-repair cream fits this profile beautifully — calm, fragrance-free, and designed to comfort rough, dry, or KP-prone skin.
You can learn more about choosing your ideal formula in Best Creams for Strawberry Skin.
3. Adjusting Daily Habits
Little changes make a huge difference for KP-prone skin:
- Keep showers short and lukewarm, not hot.
- Use gentle, fragrance-free cleansers instead of foaming body washes.
- Pat dry, don’t rub with a towel.
- Moisturize immediately after bathing while the skin is still damp.
- Avoid rough fabrics or tight clothing that cause friction.
These habits may seem small, but they make the difference between flare-ups and lasting calmness.
4. Optional Professional Treatments
If your KP feels very stubborn or textured despite consistent care, there are professional options that can complement your routine.
Chemical Peels
Dermatologists sometimes use mild acid peels to encourage cell turnover.
They can help smooth texture temporarily, but results fade without daily maintenance.
Laser Treatments
Some lasers can help reduce redness or thickened skin, but they’re not first-line treatments — and they can be pricey.
They work best when paired with consistent at-home care.
5. What Not to Do
Some popular methods make KP worse over time. Avoid:
- Harsh physical scrubs or body brushes
- Over-exfoliating (especially with acids or retinoids)
- Fragranced or alcohol-heavy lotions
- Picking or scratching bumps
Gentle care wins every time — KP improves through balance, not intensity.
How Long Does It Take to See Results?
KP doesn’t change overnight. Most people notice:
- Softer texture in 4–6 weeks
- Less redness after 6–8 weeks
- Long-term smoothing after about 3 months of consistent care
If bumps persist beyond that, it’s not that your routine isn’t working — your skin just needs time to rebuild its barrier fully.

When to See a Dermatologist
You don’t need professional care for mild KP, but it’s worth checking in if:
- Bumps become painful, red, or inflamed
- Your routine causes stinging or peeling
- You’re unsure if it’s KP or another condition
Dermatologists can confirm it and may suggest prescription-strength options or targeted exfoliants.
Can KP Go Away Completely?
Sometimes, yes — especially as you age or when you maintain a steady care routine.
For many people, KP softens significantly by their late twenties or thirties.
But even if it never fully disappears, it often becomes so mild you hardly notice it.
The key is consistency and barrier support — not chasing “perfect skin.”
If you’re curious about long-term changes, visit Does KP Go Away With Age?.
The Emotional Side of KP
It’s easy to feel self-conscious about texture, especially when it doesn’t match the smooth skin you see online.
But KP is one of the most common skin textures in the world — you’re not alone, and it’s nothing to be ashamed of.
You deserve to feel comfortable in your skin, even when it’s bumpy.
Progress, not perfection, is the real goal.
The Bottom Line
Keratosis pilaris is harmless, common, and completely manageable with patience and care.
Focus on:
- Gentle exfoliation with lactic acid or urea
- Deep daily moisture with ceramides or shea butter
- Consistent barrier protection
No harsh scrubs. No rushing. No guilt.
Just small, steady steps toward softer, calmer skin that feels like you.
To continue building your routine, explore:
FAQ: Understanding Keratosis Pilaris
Q: What causes keratosis pilaris?
A: KP happens when keratin (a protective skin protein) builds up and blocks hair follicles. Genetics, dry skin, and a weak barrier make this buildup more likely — which is why moisturizing and gentle exfoliation are the most effective long-term treatments.
Q: Is keratosis pilaris contagious or dangerous?
A: No — KP is completely harmless and not contagious. It doesn’t spread through contact or cause infection. It’s purely a texture issue, not a sign of poor hygiene or health.
Q: Does KP ever go away?
A: Often, yes. KP tends to soften or fade with age, especially when paired with consistent barrier care. For others, it may linger mildly but stay manageable through regular exfoliation and moisturizing.
Q:What’s the fastest way to smooth KP bumps?
A: There’s no instant fix — but steady, gentle care works best. Use lactic acid or urea two to three times a week, moisturize daily with ceramides or shea butter, and avoid harsh scrubs or hot showers. Visible smoothing usually starts within 4–6 weeks.





