What Triggers Eczema Flare-Ups?

You’re moisturizing, avoiding harsh soaps, and doing all the “right” things — and yet, your eczema still flares without warning. If that sounds familiar, you’re not alone.
Eczema (also known as atopic dermatitis) has a way of flaring up even when you’re being careful. That’s because it’s a condition influenced by both internal and external factors — and your skin’s threshold can change from week to week.
Understanding what tends to spark flares can help you notice patterns early, calm irritation faster, and prevent small flare-ups from turning into major ones.
For a deeper dive into eczema’s root causes and barrier issues, see Eczema Explained: Triggers, Symptoms & Treatments.
Why Flares Happen
At its core, eczema is a sign of a sensitive skin barrier. This barrier — your skin’s outermost layer — usually works like a seal to keep moisture in and irritants out.
When it’s compromised, everyday things like cold air, soap, or even stress hormones can slip past and spark inflammation. Your immune system responds with redness, dryness, and itch — what we call a “flare.”
The goal isn’t to avoid every possible trigger forever. It’s to learn which ones affect you most and keep your barrier strong enough to handle the rest.
Common Eczema Triggers
1. Dry Air and Temperature Changes
Cold, dry air is one of the most common culprits. When humidity drops, moisture evaporates from your skin more quickly, leaving it tight and irritated.
Long, hot showers and indoor heating can make things worse.
What helps:
- Short, lukewarm showers (5–10 minutes).
- Apply moisturizer immediately after bathing.
- Use a humidifier during dry seasons.
2. Harsh Soaps, Detergents, and Fragrances
Many cleansers, laundry products, and body washes contain surfactants, dyes, or perfumes that strip away natural oils. For eczema-prone skin, that can mean instant irritation.
What helps:
- Choose fragrance-free and dye-free detergents.
- Use gentle, non-foaming cleansers labeled for sensitive skin.
- Avoid fabric softeners and dryer sheets if you notice they make you itch.
3. Stress
Stress doesn’t cause eczema, but it can absolutely worsen it.
When you’re anxious, your body releases hormones that affect inflammation and barrier function. For some, that translates to an overnight flare after a tough week.
What helps:
- Build in small moments of calm: breathing, stretching, walking, or journaling.
- Keep moisturizing routines simple so care doesn’t feel like another task.
- Remember that flares during stressful periods are common and reversible.
4. Sweat and Heat
Sweating can irritate eczema-prone skin because salt from sweat stings open or sensitive areas. Overheating also dries out the skin faster.
What helps:
- Wear lightweight, breathable fabrics like cotton or bamboo.
- Rinse off and re-moisturize after workouts.
- Keep a cool compress handy during flare seasons.
5. Allergens
Environmental allergens like pollen, dust mites, mold, and pet dander can all aggravate eczema.
This doesn’t mean eczema is an “allergy,” but for some people, allergens trigger the same immune response that leads to flares.
What helps:
- Wash bedding weekly in hot water.
- Vacuum and dust regularly using a HEPA filter.
- Keep pets off the bed during flare periods if you’re sensitive.
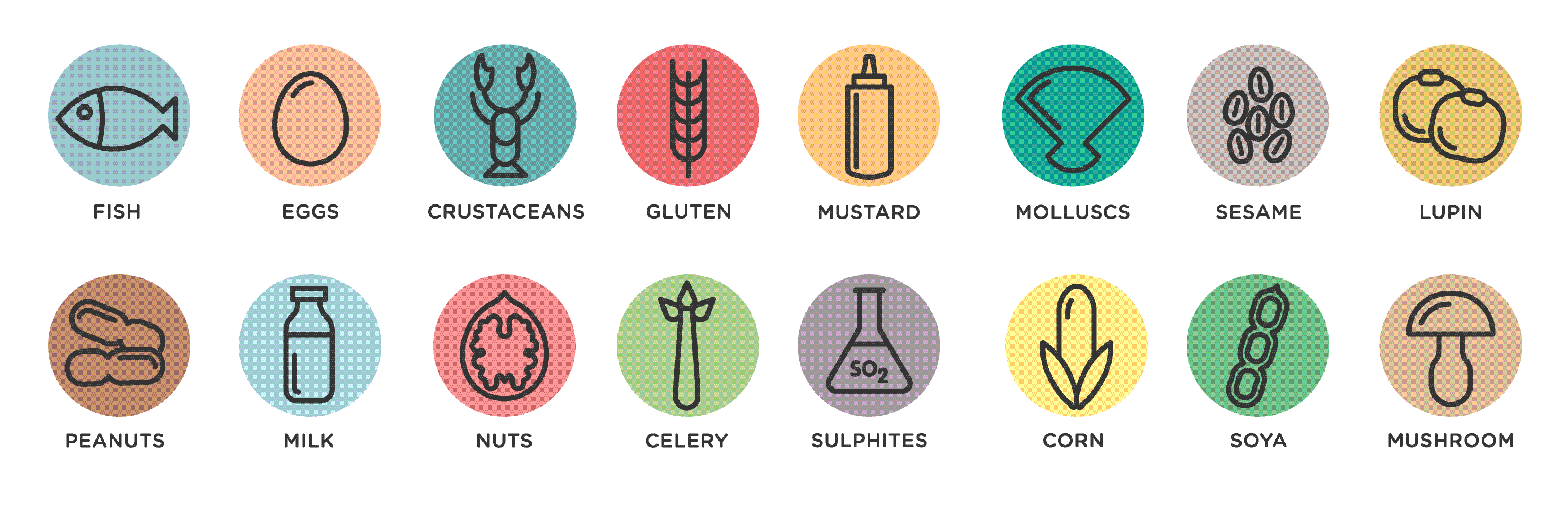
If you suspect food allergies play a role, talk to a healthcare professional before starting an elimination diet — restricting too many foods can make things worse.
6. Fabrics and Friction
Rough fabrics (like wool or stiff synthetics) can rub against the skin, causing irritation. Tight clothing traps sweat and heat, another trigger combo.
What helps:
- Stick to soft, loose, breathable fabrics.
- Wash new clothes before wearing them to remove finishing chemicals.
- Avoid tags or seams that rub against sensitive spots.
7. Infections or Illness
Colds, flu, or skin infections can all make eczema worse because the immune system is already activated.
You might notice your skin flaring during or just after being sick.
What helps:
- Keep up with regular moisturizing even when you’re unwell.
- Avoid scratching, which can open cracks for bacteria.
- If skin looks weepy, crusted, or very sore, check with a doctor to rule out infection.
8. Hormonal Shifts
Many people notice eczema changes around menstruation, pregnancy, or menopause. Fluctuating estrogen levels can affect hydration and barrier function.
What helps:
- Maintain consistent moisturizing habits even when your skin feels fine.
- Choose calming, fragrance-free products to minimize irritation during hormonal changes.
- If pregnant or breastfeeding, double-check actives like retinoids or acids with your healthcare provider before using.
Preventing Flares Before They Start
While you can’t eliminate every trigger, you can reduce how strongly your skin reacts by strengthening its barrier every day.
Core habits that help:
- Moisturize twice daily. Use a cream or ointment rich in ceramides, shea butter, and colloidal oatmeal.
- Cleanse gently. Skip foaming washes and opt for non-soap cleansers.
- Avoid temperature extremes. Keep baths warm, not hot, and protect skin from windburn.
- Stay consistent. Your skin barrier loves routine more than anything else.
Barrier-focused products — like those that blend ceramides and soothing lipids — can be especially helpful for comfort between flares. Strawberry shares several gentle guides on how to build that kind of daily eczema routine in their educational blog series.
When to Get Professional Support
If your skin is cracked, bleeding, or keeping you up at night despite regular care, reach out to a dermatologist.
They can help identify whether infections, allergies, or other conditions are contributing and may suggest prescription options.
Your moisturizer and trigger management routine will remain a foundation of care either way.
The Bottom Line
Eczema flares happen when your skin’s protective barrier meets something it can’t quite handle — whether that’s dry air, stress, or friction from clothing.
Learning your personal triggers takes time, but it’s worth it: once you know them, you can prevent many flares before they begin.
Keep things simple, gentle, and consistent.
And remember — every small choice that supports your barrier brings you one step closer to calmer, more comfortable skin.
References:
- National Eczema Association – Common Triggers
- American Academy of Dermatology – Eczema Management Tips
- National Institutes of Health – Atopic Dermatitis Overview.
FAQ: Understanding and Managing Eczema Flare Triggers
Why do my eczema flares happen even when I’m careful?
Because eczema isn’t caused by just one thing. It’s influenced by both internal and external factors — like stress, weather, hormones, or allergens. Even when you’re doing everything “right,” your skin barrier’s threshold can shift from week to week, making it more reactive at times.
What are the most common eczema triggers?
The most frequent triggers include dry air, harsh soaps, stress, sweat, allergens, and friction from clothing. Infections or hormonal changes can also worsen symptoms. Tracking your flares with a simple skin diary can help pinpoint which factors affect you most.
Can stress alone cause a flare?
Stress doesn’t directly cause eczema, but it can intensify it. Stress hormones can weaken the skin barrier and raise inflammation levels, making your skin more sensitive. Gentle stress management — walks, journaling, or breathing exercises — can noticeably reduce flare frequency.
How can I prevent flare-ups long term?
Consistency is key. Keep your skin barrier strong by:
- Moisturizing twice daily with ceramide-rich creams.
- Using fragrance-free cleansers and detergents.
- Avoiding extreme temperatures.
- Managing stress and getting adequate sleep.
A strong barrier is your skin’s best defense against future flares.





